Betapace vs Alternatives: Medication Comparison Tool
This interactive tool helps compare Betapace (Sotalol) with its major alternatives for treating heart rhythm disorders. Select a medication below to see detailed information about its use, benefits, and considerations.
Mechanism: Class III anti-arrhythmic with beta-blocking properties. Slows heart rate and prolongs cardiac action potential.
Uses: Maintaining sinus rhythm after cardioversion for atrial fibrillation and preventing ventricular tachycardia.
Dosing: Starts at 80 mg twice daily, up to 320 mg twice daily depending on renal function.
Monitoring: Baseline ECG required; QTc interval checked frequently due to risk of torsades de pointes.
Special Considerations: Dose adjustments needed in CKD. Half-life of 12-20 hours allows twice-daily dosing.
| Feature | Betapace | Amiodarone | Dofetilide | Flecainide | Propafenone | Metoprolol |
|---|---|---|---|---|---|---|
| Class | Class III + Beta-blocker | Class III + Multi-channel blocker | Class III | Class IC | Class IC | Beta-blocker |
| Main Use | Rhythm control | Refractory VT | Rhythm control | Rhythm control | Rhythm control | Rate control |
| Monitoring Needs | QTc monitoring | Regular labs (liver, thyroid) | Daily ECG | ECG monitoring | ECG monitoring | Basic monitoring |
| Side Effects | QT prolongation, bradycardia | Thyroid dysfunction, lung issues | QT prolongation | Heart failure risk | Heart failure risk | Bradycardia, fatigue |
Choosing the right medication for irregular heartbeats can feel like navigating a maze. Betapace (the commercial name for sotalol) sits at the intersection of beta‑blockers and classIII anti‑arrhythmics, which makes it a popular option for many patients with atrial fibrillation or ventricular arrhythmias. But it isn’t the only game in town. This guide breaks down how Betapace works, how it stacks up against the most common alternatives, and what factors should tip the scales in favour of one drug over another.
TL;DR
- Betapace combines beta‑blocking and potassium‑channel blocking, useful for both atrial fibrillation and ventricular arrhythmias.
- Amiodarone is the most potent anti‑arrhythmic but carries long‑term organ toxicity.
- Dofetilide, Flecainide, and Propafenone are classIII or classIC agents with specific dosing and monitoring needs.
- Metoprolol offers pure beta‑blockade; it’s safer for rate control but doesn’t terminate arrhythmias.
- Choose based on rhythm vs rate control goals, organ health, and ability to monitor QT interval.
What is Betapace (Sotalol) and How Does It Work?
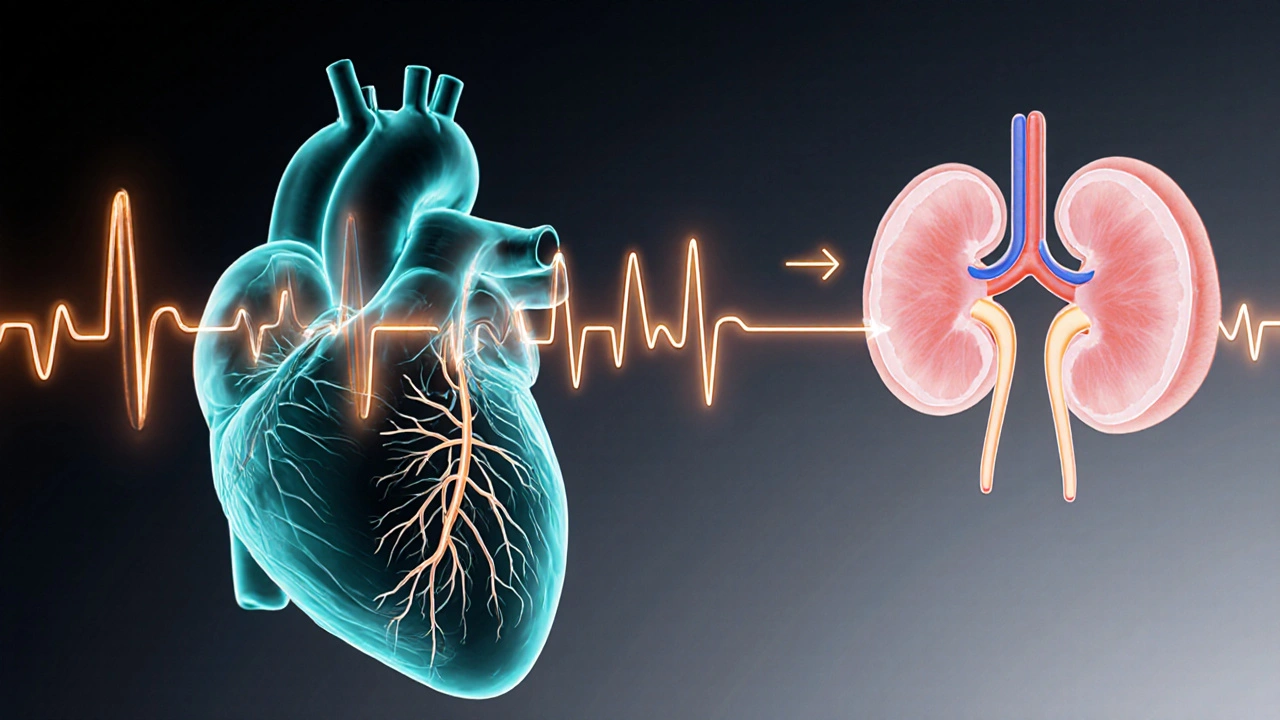
Betapace is the brand name for sotalol, a classIII anti‑arrhythmic that also blocks beta‑adrenergic receptors. Its dual action means it slows heart‑rate (beta‑blockade) while prolonging the cardiac action potential (potassium‑channel blockade). This combination is effective in maintaining sinus rhythm after cardioversion for atrial fibrillation and in preventing recurrent ventricular tachycardia.
Typical oral dosing starts at 80mg twice daily, with titration up to 320mg twice daily depending on renal function and QT interval. Because sotalol is excreted unchanged by the kidneys, dose adjustment is crucial in chronic kidney disease (CKD). The drug’s half‑life ranges from 12 to 20hours, allowing twice‑daily dosing.
Monitoring focuses on the QTc interval. A baseline ECG is required, followed by checks at 2‑4hours after the first dose, then daily for the first three days, and weekly until the dose stabilises. QTc >500ms or an increase >60ms signals a high risk for torsades de pointes, prompting dose reduction or discontinuation.
Major Alternatives to Betapace
The anti‑arrhythmic landscape includes several agents that target similar rhythm disorders but differ in mechanism, side‑effect profile, and monitoring burden.
Amiodarone
Amiodarone is a classIII anti‑arrhythmic with a broad spectrum of activity, affecting potassium, sodium, calcium channels and beta receptors. It is the go‑to drug for refractory ventricular tachycardia and for patients who cannot tolerate other agents. Dosing usually starts with a loading phase of 800‑1200mg daily for 1‑2weeks, then a maintenance dose of 100‑200mg daily.
Amiodarone’s major drawback is its long half‑life (up to 60days) and multi‑organ toxicity-thyroid dysfunction, pulmonary fibrosis, hepatic injury, and skin discoloration. Routine labs (TSH, liver enzymes, chest X‑ray) are required every 3‑6months.
Dofetilide
Dofetilide is a pure classIII potassium‑channel blocker approved for maintenance of sinus rhythm in atrial fibrillation and flutter. Initiation must occur in a hospital setting because of a high incidence of QT‑prolongation. Starting doses range from 125‑500µg twice daily, adjusted for creatinine clearance.
Because it carries a similar torsades risk to sotalol, daily ECG monitoring for the first 3 days is mandatory. Renal function dictates dose; patients with CrCl<20mL/min are generally excluded.
Flecainide
Flecainide is a classIC sodium‑channel blocker used for 'pill‑in‑the‑pocket' conversion of paroxysmal atrial fibrillation and for certain ventricular arrhythmias. Oral dosing is 200‑300mg as a single dose for conversion, or 50‑100mg twice daily for maintenance.
Flecainide is contraindicated in structural heart disease, coronary artery disease, and heart failure because it can be pro‑arrhythmic. Baseline ECG and careful assessment of QRS width are essential.
Propafenone
Propafenone is another classIC agent that also has mild beta‑blocking activity, offering rhythm control with some rate‑control benefit. Doses are similar to flecainide: 600mg single‑dose for conversion or 150‑300mg twice daily for maintenance.
Like flecainide, propafenone should be avoided in patients with left‑ventricular dysfunction or prior myocardial infarction. Monitoring focuses on QRS duration and signs of bradycardia.
Metoprolol
Metoprolol is a selective β‑1 blocker used primarily for rate control in atrial fibrillation and for secondary prevention after myocardial infarction. While it does not terminate arrhythmias, it helps control ventricular response and reduces sympathetic trigger.
Typical dosing is 25‑100mg twice daily (immediate‑release) or 50‑200mg once daily (extended‑release). Side effects include fatigue, cold extremities, and in rare cases, bronchospasm in asthmatics.
Side‑Effect Summary Across Drugs
- Betapace (Sotalol): Bradycardia, hypotension, torsades de pointes, fatigue.
- Amiodarone: Thyroid disease, pulmonary fibrosis, liver enzyme elevation, photosensitivity.
- Dofetilide: QT prolongation, torsades, renal‑related dose adjustments.
- Flecainide: Pro‑arrhythmia in structural heart disease, visual disturbances.
- Propafenone: Similar to flecainide plus mild beta‑blockade side effects.
- Metoprolol: Bradycardia, fatigue, potential worsening of asthma.
Comparison Table
| Drug | Class | Primary Indication | Dose Range (oral) | Half‑life | Major Toxicities | Monitoring |
|---|---|---|---|---|---|---|
| Betapace (Sotalol) | ClassIII + β‑blocker | Atrial fibrillation, ventricular tachycardia | 80‑320mg BID | 12‑20h | QT prolongation, bradycardia | Baseline & serial ECG, renal function |
| Amiodarone | ClassIII (multi‑channel) | Refractory VT/VF, AF | 800‑1200mg loading, 100‑200mg maintenance | Up to 60days | Thyroid, lung, liver, skin | TSH, LFTs, chest X‑ray, ECG |
| Dofetilide | ClassIII | AF/flutter maintenance | 125‑500µg BID (CrCl‑adjusted) | 10‑12h | QT prolongation, torsades | In‑hospital ECG for 3days, renal function |
| Flecainide | ClassIC | Paroxysmal AF conversion, VT | 200‑300mg single; 50‑100mg BID | 12‑20h | Pro‑arrhythmia in CAD/CHF | QRS width, avoid structural disease |
| Propafenone | ClassIC (+β‑blockade) | AF conversion & maintenance | 600mg single; 150‑300mg BID | 12‑20h | Similar to flecainide, bronchospasm | QRS, bronchial assessment |
| Metoprolol | β‑1 blocker | Rate control in AF, post‑MI | 25‑100mg BID or 50‑200mg QD ER | 3‑7h | Bradycardia, fatigue, asthma risk | Pulse, blood pressure, symptom review |
How to Choose the Right Drug for You
Deciding between Betapace and its rivals boils down to three clinical questions:
- Do you need rhythm control (restore/maintain sinus rhythm) or just rate control? If you only need to slow the heart, a pure beta‑blocker like Metoprolol is simpler and safer.
- What is the patient’s organ health? Renal impairment steers you away from sotalol and dofetilide; liver or thyroid disease makes amiodarone risky.
- Can you meet the monitoring requirements? Sotalol and dofetilide need daily ECGs early on; amiodarone demands long‑term lab surveillance.
Here’s a quick decision matrix:
- Kidney function normal, wants rhythm control, can handle ECG monitoring → Betapace or Dofetilide.
- Structural heart disease present, needs rhythm control → Avoid Flecainide/Propafenone; consider Amiodarone.
- History of thyroid or lung disease → Prefer Betapace or a beta‑blocker over Amiodarone.
- Only rate control needed, low monitoring capacity → Metoprolol or other β‑blockers.
Practical Checklist for Clinicians & Patients
- Confirm indication (AF vs VT) and therapeutic goal (rate vs rhythm).
- Assess renal, hepatic, thyroid, and pulmonary status before picking a drug.
- Obtain baseline ECG; calculate QTc.
- Choose initial dose according to guidelines and patient weight.
- Schedule ECGs: 2‑4h post‑first dose, then daily for 3days (Betapace/Dofetilide).
- Educate patient on symptoms of torsades: palpitations, dizziness, fainting.
- Arrange follow‑up labs: electrolytes, TSH (if amiodarone), liver enzymes.
- Document any dose adjustments and reasons in the medical record.

Frequently Asked Questions
Can I switch from Betapace to another anti‑arrhythmic without a wash‑out period?
A short overlap is usually safe if the new drug has a different mechanism and you monitor the QT interval closely. For example, transitioning to amiodarone often requires a 24‑hour overlap while checking electrolytes, whereas moving to a pure β‑blocker like metoprolol can be done the next day after confirming heart rate control.
Why does sotalol cause both beta‑blockade and QT prolongation?
Sotalol’s molecular structure fits both the β‑adrenergic receptor pocket (blocking sympathetic stimulation) and the cardiac potassium channel (delaying repolarisation). This dual effect is rare among anti‑arrhythmics and gives it unique utility-but also raises the risk of bradycardia plus torsades if dosing isn’t carefully titrated.
Is Betapace safe for older adults with mild kidney decline?
If creatinine clearance is above 50mL/min, standard dosing is usually fine. Below that, the dose should be halved, and ECG monitoring becomes more frequent. Many clinicians avoid sotalol altogether if CrCl drops under 30mL/min.
How does amiodarone’s long half‑life affect treatment planning?
Because the drug sticks around for weeks, any side‑effects can persist long after stopping. Physicians often start with a loading dose to achieve therapeutic levels quickly, then shift to a low maintenance dose to minimise organ toxicity. Patients need lifelong lab surveillance even if the drug appears to work.
When is “pill‑in‑the‑pocket” therapy appropriate?
For patients with infrequent, symptomatic AF episodes and no structural heart disease, a single dose of flecainide or propafenone taken at onset can convert rhythm without daily medication. This approach avoids chronic side‑effects but requires clear patient education on when to seek emergency care.