Why Do Pills Cost So Much More in Some Countries?
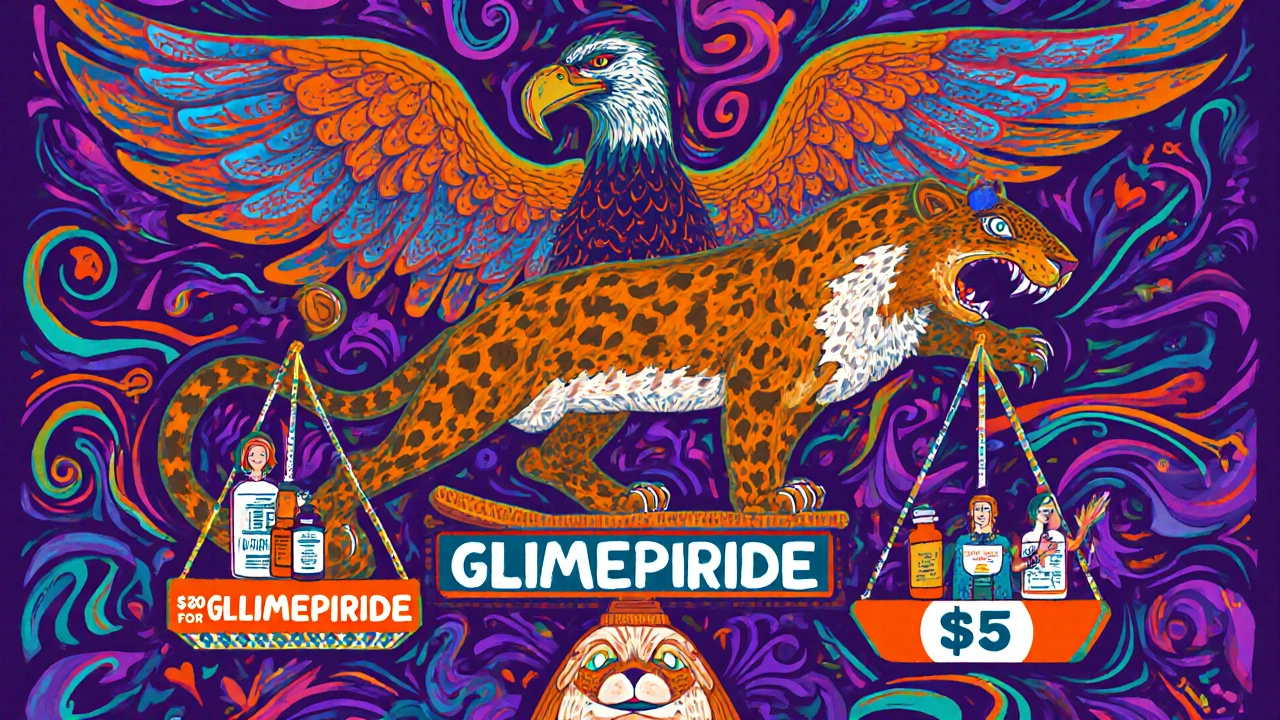
If you’ve ever compared the price of your prescription at home versus abroad, you know something’s off. A month’s supply of glimepiride might cost $5 in Canada but $80 in the U.S. And then there’s Ozempic - one of the most talked-about drugs today - priced at over $1,000 in America but under $300 in Australia. It’s not about quality. It’s not about manufacturing. It’s about policy.
The U.S. doesn’t negotiate drug prices like most other wealthy nations. Instead, it lets pharmaceutical companies set list prices, then relies on insurers and pharmacy benefit managers to negotiate discounts behind closed doors. Meanwhile, countries like Germany, Japan, and Australia use government-backed price controls, reference pricing, and direct negotiations to keep costs down. The result? Wildly different bills at the pharmacy counter - even for the exact same pill.
The U.S. Pays More - But Only for Brand-Name Drugs
It’s easy to say the U.S. pays the most for drugs. And it’s true - but only if you’re looking at brand-name medications. According to the U.S. Department of Health and Human Services, U.S. list prices for originator drugs are 278% higher than in other OECD countries. For newer biologics like Enbrel or Stelara, that gap widens to over 400%.
But here’s what most people miss: 90% of prescriptions filled in the U.S. are for generics. And guess what? Generic drugs in the U.S. cost 67% less than in other countries. That’s because U.S. pharmacies and insurers have powerful leverage over generic manufacturers. The result? A dual system: sky-high prices for new drugs, rock-bottom prices for old ones.
Take Jardiance, a diabetes drug. In Japan, it costs $52 per month. In the U.S., before Medicare negotiations, it was $204. But the generic version of a similar drug, metformin, costs less than $5 a month in both places. So while Americans pay more for innovation, they pay less for basics.
How Other Countries Keep Prices Low
Most developed countries don’t let drugmakers set their own prices. They have systems in place to control costs.
- Japan uses a national price schedule updated every two years. If a drug is priced higher than similar ones, it gets cut. That’s why Japan consistently has the lowest prices for drugs like Entresto and Imbruvica.
- France and Germany use external reference pricing - they look at what other countries pay and cap their own prices accordingly. If Australia pays $300 for a drug, France won’t pay more than that.
- Australia has the Pharmaceutical Benefits Scheme (PBS). The government negotiates directly with companies. If the price isn’t fair, the drug doesn’t get listed. That’s why Eliquis, Xarelto, and Farxiga are cheapest in Australia.
- Canada uses the Patented Medicine Prices Review Board to ensure prices aren’t “excessive.” Even so, Canada still pays more than most European countries because it doesn’t always match the lowest global prices.
These systems aren’t perfect. Sometimes patients wait longer for new drugs. But overall, they keep out-of-pocket costs manageable for millions.

Medicare’s New Power to Negotiate - And What It Means
In 2022, the U.S. passed the Inflation Reduction Act. For the first time, Medicare gained the right to negotiate prices for a small number of high-cost drugs. The first 10 were announced in 2023, with prices taking effect in 2025.
Here’s what happened:
- Jardiance: Medicare negotiated a price of $204 - still 3.9 times higher than Japan’s $52.
- Stelara: $4,490 for Medicare vs. $2,822 in other countries - still 1.6 times higher.
- Ozempic: Even though it’s one of the top-selling drugs in Medicare Part D, its negotiated price is still far above what other countries pay.
Medicare’s negotiated prices are lower than what private insurers used to pay - but they’re still much higher than international benchmarks. In nearly half of the cases, Medicare’s price was more than three times what other countries pay.
And here’s the kicker: Medicare is required to pick 15 more drugs for negotiation by February 1, 2025. That means more price drops ahead - but only for a handful of expensive drugs. Most Americans will still pay full list price unless their insurer negotiates separately.
Global Price Differences Are Even Wilder Than You Think
It’s not just rich countries. A 2024 study in JAMA Health Forum looked at 549 essential medicines across 72 countries - and adjusted for how much people actually earn. That’s called purchasing power parity.
The results were shocking:
- In Lebanon, the price of essential medicines was just 18% of Germany’s baseline.
- In Argentina, prices were nearly six times higher than in Germany.
- In the Western Pacific (including Australia, China, Japan), median prices were the lowest globally.
- In the Americas, median prices were the highest - nearly 65% above the global average.
This isn’t just about wealth. It’s about policy. Countries with strong public health systems and centralized buying power keep prices low. Countries without them - even wealthy ones - pay more.

Why the U.S. System Makes Sense - If You’re a Drug Company
Some economists argue the U.S. system isn’t broken - it’s working as designed. The idea? High prices for new drugs fund innovation. Lower prices for generics keep daily meds affordable.
According to researchers at the University of Chicago, the U.S. model balances two goals: access to cheap generics and funding for breakthroughs. The U.S. is home to most of the world’s top pharmaceutical R&D. Without high prices on new drugs, they argue, those innovations wouldn’t happen.
But here’s the problem: The U.S. isn’t the only country funding innovation. Germany, Switzerland, and Japan also have strong pharma industries. And they pay far less for the same drugs. So why does the U.S. shoulder so much of the cost? It’s not because American patients need more innovation - it’s because the system lets drugmakers charge whatever they want.
As one analyst put it: "Americans are subsidizing global drug development - and they’re running out of patience."
What This Means for You
If you’re in the U.S. and struggling to afford your meds:
- Ask if there’s a generic version - even if your doctor didn’t suggest it.
- Check GoodRx or RxSaver - they often show prices lower than your insurance copay.
- For expensive drugs like Ozempic or Humira, look into patient assistance programs. Many drugmakers offer them.
- If you’re on Medicare, keep an eye on the 2025 negotiated drug list. You might see a big drop in your bill.
If you’re outside the U.S., you’re likely paying less - but you might wait longer for new drugs. That trade-off - lower cost vs. faster access - is the real story behind global drug pricing.
What’s Next?
By 2026, Medicare will be negotiating 15 more drugs. More countries will tighten their price controls. Generic manufacturers will keep pushing prices down. But the big question remains: Will the U.S. ever adopt a system like Australia’s or Japan’s?
For now, the answer is no. But with inflation, political pressure, and public outrage growing, the status quo won’t last forever. The next few years will show whether America chooses to join the rest of the world - or keeps paying the highest price on Earth.
Why are drug prices so much higher in the U.S. than in other countries?
The U.S. doesn’t have government price controls like most other wealthy nations. Drugmakers set list prices, and private insurers negotiate discounts behind the scenes. Other countries, like Japan and Australia, use direct government negotiation or reference pricing - meaning they cap prices based on what other countries pay. This gives them far more leverage to keep costs low.
Are generic drugs cheaper in the U.S. than elsewhere?
Yes. Generic drugs in the U.S. cost about 67% less on average than in other developed countries. That’s because U.S. pharmacies and insurers have massive buying power and can pressure generic manufacturers to offer deep discounts. The U.S. fills 90% of prescriptions with generics - far more than most other nations - which helps keep overall spending lower despite high brand-name prices.
Which country has the lowest drug prices?
Japan consistently has the lowest prices for most brand-name drugs, including Jardiance, Entresto, and Imbruvica. Australia often has the lowest prices for drugs like Eliquis and Xarelto. Both countries use aggressive government negotiation and price caps. France and Germany also rank among the lowest, though slightly higher than Japan.
Does Medicare’s new drug negotiation mean my prices will drop?
Only if you take one of the 10 drugs Medicare negotiated in 2023 - and only if you’re on Medicare Part D. The first price drops took effect in January 2025. For most Americans, prices won’t change unless your insurer negotiates separately. The next round of 15 drugs will be announced in February 2025, so more savings could be coming.
Why do some countries have trouble getting new drugs?
Countries with strict price controls often delay approving new drugs until they’ve negotiated a fair price. This can mean waiting months or even years for a new medication to become available. The U.S. gets new drugs faster - but at a much higher cost. It’s a trade-off: speed vs. affordability.
Can I legally buy cheaper drugs from other countries?
Technically, importing prescription drugs from other countries is against U.S. law - but enforcement is rare for personal use. Many Americans buy medications from Canada, Mexico, or India through online pharmacies. While this carries some risk (like counterfeit drugs), many people do it to save hundreds or thousands of dollars. Always check if the pharmacy is verified and consult your doctor before switching sources.
Is the U.S. system better for drug innovation?
The U.S. funds more drug research than any other country, but it’s not because it pays the most. Most new drugs are developed by U.S. companies - but they’re sold globally. Other countries pay less, but still buy the drugs. So the U.S. isn’t the only one subsidizing innovation. In fact, many experts argue the U.S. pays far more than necessary to fund R&D, and that other countries could afford to pay more without hurting access.