Blood Pressure Medication Comparison Tool
Personalized Blood Pressure Medication Advisor
Answer a few questions to determine which blood pressure medication might be most suitable for your specific health profile.
High blood pressure is a silent culprit that can lead to heart attacks, strokes, and kidney damage if left unchecked. Many people start their treatment with Prinivil, but the market is full of other options that might fit a different lifestyle, budget, or health profile. This guide walks through how Prinivil works, its strengths and drawbacks, and how it stacks up against the most common alternatives.
Key Takeaways
- Prinivil (lisinopril) is an ACE inhibitor that lowers blood pressure by relaxing blood vessels.
- Typical side effects include cough, dizziness, and elevated potassium.
- Alternatives span three major classes: other ACE inhibitors, ARBs, and calcium‑channel blockers.
- Cost, kidney function, and risk of cough are the top factors when choosing a medication.
- Consult your doctor before switching, especially if you have diabetes or chronic kidney disease.
What Is Prinivil (Lisinopril)?
Prinivil is a brand name for lisinopril, an angiotensin‑converting enzyme (ACE) inhibitor approved by the FDA in 1987. It belongs to the ACE inhibitor class, which blocks the conversion of angiotensin I to the vasoconstrictor angiotensin II. By doing so, blood vessels relax, blood pressure drops, and the heart works less hard.
Typical adult dosing starts at 10mg once daily, with a common maintenance range of 20-40mg. The drug’s half‑life is about 12hours, allowing once‑daily dosing for most patients. In Australia, a 30‑day supply costs roughly AU$30-$45, depending on the pharmacy.
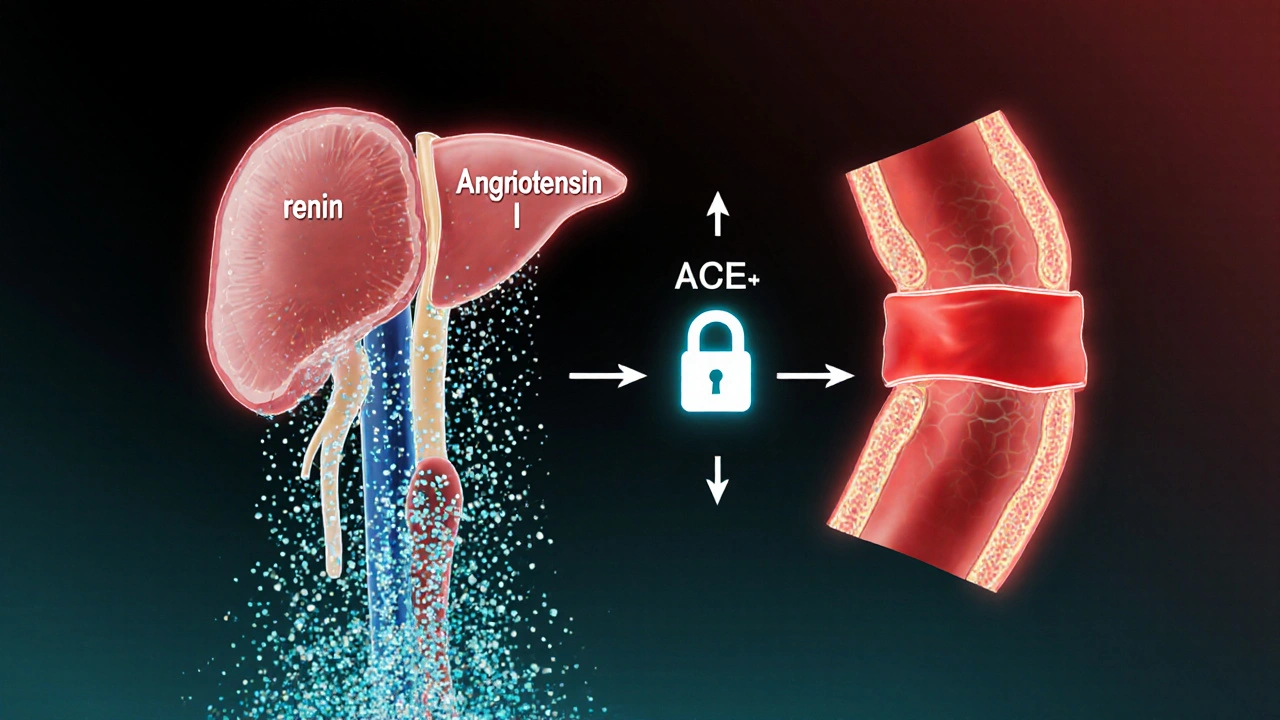
How Prinivil Works - A Quick Mechanism
The renin‑angiotensin‑aldosterone system (RAAS) regulates blood pressure. When blood volume drops, kidneys release renin, which converts angiotensinogen to angiotensin I. ACE then turns angiotensin I into angiotensin II, a potent vasoconstrictor that also triggers aldosterone release, causing sodium and water retention.
Lisinopril interferes at the ACE step, reducing angiotensinII levels. The result is lower vascular resistance, decreased sodium retention, and ultimately lower systolic and diastolic pressures.
Pros and Cons of Prinivil
- Pros
- Proven efficacy - large clinical trials show 10‑15mmHg average reduction in systolic pressure.
- Once‑daily dosing simplifies adherence.
- Low cost compared with many newer agents.
- Beneficial for patients with heart failure or post‑myocardial‑infarction.
- Cons
- Dry cough occurs in 5‑10% of users, sometimes leading to discontinuation.
- Not ideal for people with high potassium or severe kidney disease.
- May cause angio‑edema, though rare.
- Interactions with NSAIDs can blunt blood‑pressure‑lowering effect.
Common Alternatives to Prinivil
When Prinivil’s side‑effects or contraindications become an issue, physicians often turn to drugs from three major families.
- Ramipril - another ACE inhibitor with a slightly longer half‑life (13hours) and a once‑daily dose of 2.5‑10mg. Some patients tolerate it better than lisinopril, though cough rates are similar.
- Losartan - an angiotensinII receptor blocker (ARB) that blocks the hormone’s action instead of its production. Typical dose 50‑100mg daily, fewer cough complaints, but a modest increase in potassium.
- Amlodipine - a calcium‑channel blocker that relaxes arterial smooth muscle. Daily dose 5‑10mg, useful for patients with isolated systolic hypertension, but can cause peripheral edema.
- Metoprolol - a beta‑blocker that reduces heart rate and cardiac output. Doses range 50‑200mg, helpful post‑MI, yet may worsen asthma.
Side‑by‑Side Comparison
| Medication | Class | Typical Dose | Mechanism | Common Side Effects | Approx. Monthly Cost (AU$) |
|---|---|---|---|---|---|
| Prinivil (Lisinopril) | ACE Inhibitor | 10‑40mg daily | Blocks ACE → ↓ AngiotensinII | Cough, dizziness, elevated K⁺ | 30‑45 |
| Ramipril | ACE Inhibitor | 2.5‑10mg daily | Blocks ACE → ↓ AngiotensinII | Cough, fatigue, rash | 35‑50 |
| Losartan | ARB | 50‑100mg daily | Blocks AT₁ receptor → ↓ AngiotensinII effect | Elevated K⁺, dizziness | 45‑60 |
| Amlodipine | Calcium‑Channel Blocker | 5‑10mg daily | Inhibits Ca²⁺ influx in vascular smooth muscle | Edema, flushing, headache | 40‑55 |
| Metoprolol | Beta‑Blocker | 50‑200mg daily | Blocks β₁ receptors → ↓ heart rate | Bradycardia, fatigue, sexual dysfunction | 30‑45 |
Choosing the Right Medication - Decision Criteria
Picking a blood‑pressure drug isn’t a one‑size‑fits‑all exercise. Below are the most common factors patients should weigh, along with a quick checklist.
- Kidney function - ACE inhibitors and ARBs can raise potassium; if eGFR <30mL/min, a calcium‑channel blocker may be safer.
- Cough tolerance - a persistent dry cough points away from ACE inhibitors toward an ARB.
- Cost and insurance coverage - generic lisinopril and metoprolol are usually cheapest; newer brand‑names may need co‑pay.
- Comorbid conditions
- Heart failure - ACE inhibitors or beta‑blockers are first‑line.
- Diabetes - ACE inhibitors or ARBs protect kidney health.
- Asthma - Avoid non‑selective beta‑blockers.
- Lifestyle preferences - once‑daily dosing (lisinopril, ramipril, losartan) beats twice‑daily regimens for some patients.
Ask your doctor to run a basic blood panel (creatinine, potassium) before starting or switching. Most clinicians will schedule a follow‑up after 2‑4weeks to assess blood‑pressure response and side‑effects.
Frequently Asked Questions
Can I switch from Prinivil to an ARB without a washout period?
Yes, most doctors advise a direct switch because both classes act on the RAAS. However, a short monitoring window (1‑2weeks) helps catch any rise in potassium.
Why does Prinivil cause a cough?
ACE inhibitors increase bradykinin levels in the lungs, which irritates airway nerves and triggers a dry cough in a subset of patients.
Is a higher dose of Prinivil more effective?
Blood‑pressure response plateaus around 20‑40mg daily. Going beyond 40mg rarely adds benefit but raises side‑effect risk.
Can I take Prinivil with my over‑the‑counter NSAID?
Occasional NSAID use is okay, but chronic use can blunt the blood‑pressure‑lowering effect and increase kidney stress. Discuss long‑term NSAID plans with your GP.
Which medication is best for a 70‑year‑old with mild kidney disease?
A low‑dose ARB like losartan or a calcium‑channel blocker such as amlodipine is often preferred, as they carry less risk of raising potassium compared with ACE inhibitors.
Bottom line: Prinivil remains a solid first‑line choice for many adults with hypertension, but the decision should balance efficacy, side‑effects, kidney health, and cost. Talk to your healthcare provider about which alternative aligns best with your personal health profile.