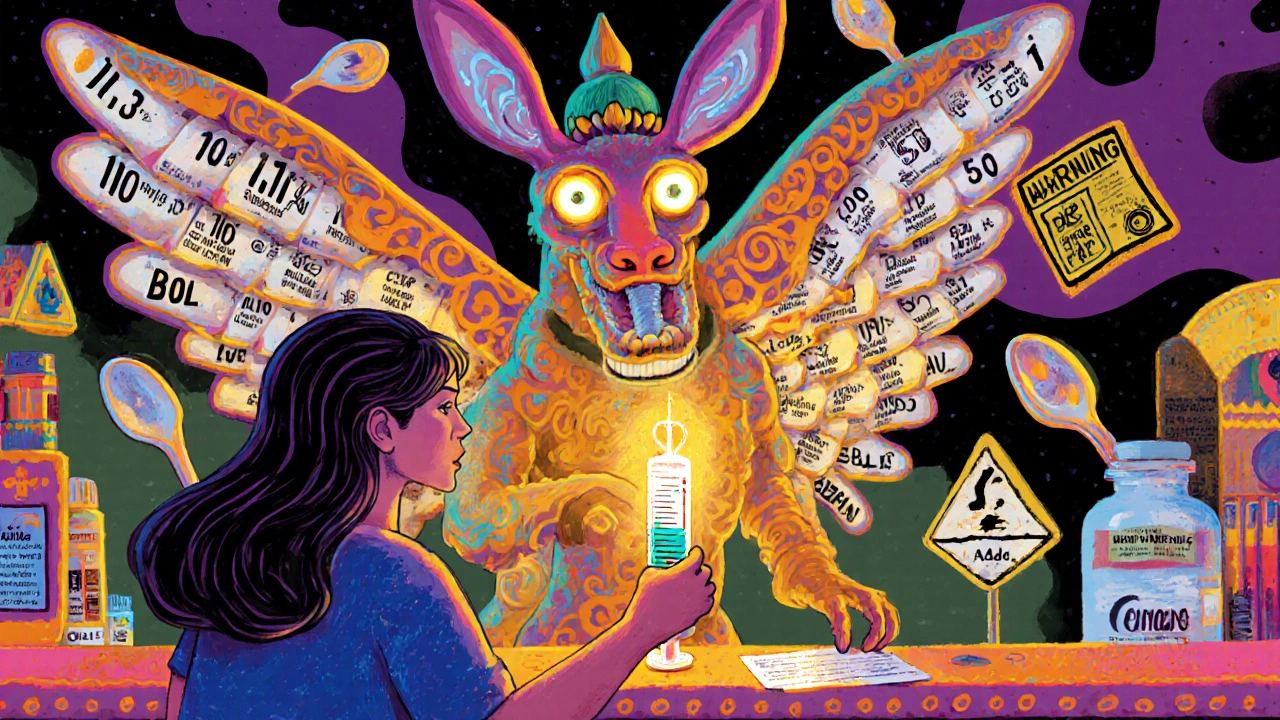
Medication Strength Verification: How to Confirm Dosage Accuracy and Avoid Dangerous Mistakes
When you pick up a prescription, medication strength verification, the process of confirming the exact dose and form of a drug matches what was prescribed. It's not just a pharmacy formality—it’s your last line of defense against a dangerous mistake. A 10mg pill isn’t the same as a 50mg pill. A tablet isn’t the same as a capsule with the same name. And a generic version? It might look totally different but still be safe—if verified correctly.
Pharmacists don’t just count pills. They check the drug formulation, the physical and chemical structure of the medication, including its strength, release type, and inactive ingredients, compare it to the prescriber’s order, and cross-reference it with your history. Medication errors, preventable mistakes in prescribing, dispensing, or taking drugs are one of the top causes of preventable harm in healthcare. Many happen because someone assumed the pill looked right, or didn’t question why the color changed. That’s why medication strength verification matters more than ever—especially with rising generic use, compounded drugs, and complex regimens.
It’s not just about pills. Liquid meds can be mixed wrong. Transdermal patches can be mislabeled. Even insulin pens vary in strength. That’s why you need to know what to look for: pill imprint codes, bottle labels, color changes, and how the pharmacy communicates changes. You’re not being difficult if you ask, "Is this the same strength as last time?" You’re being smart. The posts below show real cases where strength mix-ups happened—like warfarin and antibiotics affecting INR levels, or compounded meds with unclear beyond-use dates—and how people caught them before it was too late. You’ll see how pharmacists use databases to verify strength, what questions to ask your provider, and how to spot red flags in your own meds. This isn’t theory. It’s what keeps you alive.