Precision Medicine: Personalized Treatments Based on Your Genetics and Lifestyle
When you hear precision medicine, a healthcare approach that customizes treatment based on an individual’s genes, environment, and lifestyle. Also known as personalized medicine, it moves away from the old one-size-fits-all model and asks: What works best for you? This isn’t science fiction — it’s happening right now in cancer clinics, heart disease programs, and even in how doctors choose your next antidepressant or blood thinner.
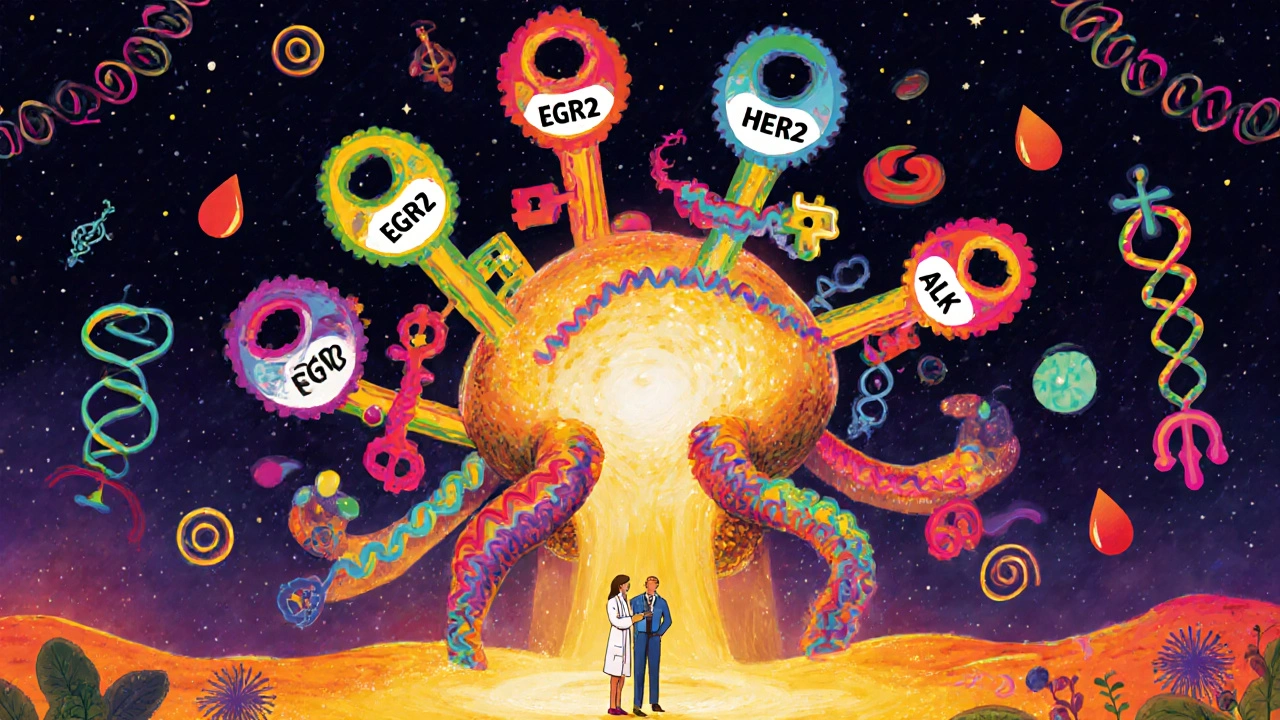
At its core, precision medicine, a healthcare approach that customizes treatment based on an individual’s genes, environment, and lifestyle. Also known as personalized medicine, it moves away from the old one-size-fits-all model and asks: What works best for you? relies on three big pieces: your DNA, your health history, and how your body reacts to drugs. For example, some people break down warfarin slowly — too much and they bleed; too little and they clot. Genetic tests can tell your doctor exactly how much to give you. That’s pharmacogenomics, the study of how genes affect a person’s response to drugs. Also known as drug-gene interaction analysis, it helps avoid dangerous side effects before they happen. Same goes for cancer: instead of giving everyone the same chemo, doctors now test tumors for specific mutations and match them to drugs that target those exact flaws. It’s like using a key that fits only one lock — fewer side effects, better results.
It’s not just about genes, though. Your diet, sleep, stress levels, and even where you live play a role. That’s why precision medicine also looks at lifestyle patterns. If you have restless legs syndrome, for instance, your doctor might check your iron levels before prescribing dopamine drugs — because low iron makes those meds less effective and riskier. Or if you’re on opioids long-term, they might test your adrenal function — because those drugs can silently shut down your body’s stress response. This isn’t guesswork. It’s data-driven care.
And it’s not just for the sick. Precision medicine helps prevent disease before it starts. If your family has a history of heart problems, a simple genetic screen might show you’re at higher risk — so you can start lifestyle changes early, or choose a blood pressure med that works better for your biology. It’s why you’re seeing more labs offering at-home DNA kits, and why doctors are asking more about your meds, your diet, and your sleep.
What you’ll find below isn’t a list of buzzwords. It’s real-world examples of precision medicine in action: how genetic testing changes how we treat alcohol dependence, why some people get delirium from antibiotics while others don’t, how drug interactions like warfarin and antibiotics are now predicted before they happen, and how knowing your body’s unique chemistry helps you avoid dangerous side effects. These aren’t theoretical studies — they’re stories of people who got the right drug, at the right dose, at the right time — because their care was built around them, not the other way around.