Medication Side Effect Timeline Estimator
How Soon Might Side Effects Appear?
Enter your medication type and personal details to estimate when you might experience side effects based on clinical data.
Critical Time Windows
Key Warning Signs By Timeframe
Critical Warning Signs
Call your doctor immediately if you experience:
- Swelling of face, lips, or tongue
- Rash with fever or blisters
- Yellow skin or eyes
- Severe muscle pain
- Difficulty breathing
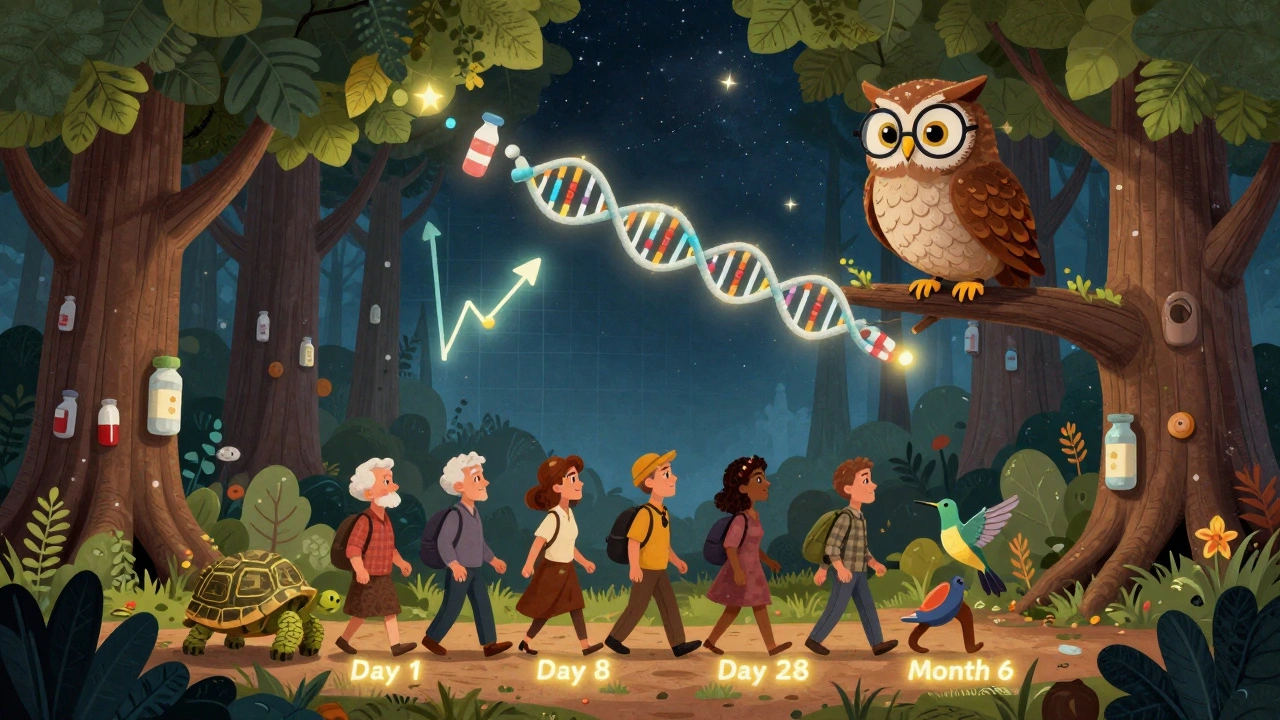
When you start a new medication, it’s natural to wonder: when will the side effects show up? And if they do, how do you know if it’s just your body adjusting-or something serious? The answer isn’t the same for every drug. Some reactions hit within minutes. Others creep in weeks later. Knowing the typical timeline can help you spot trouble early, avoid panic, and talk smarter with your doctor.
Immediate Reactions: Minutes to One Hour
If something bad happens right after you take a pill, it’s usually an allergic or hypersensitivity reaction. These are fast. Anaphylaxis, the most dangerous type, can start in under 15 minutes. About 67% of cases begin this quickly, according to emergency room data from the American Academy of Allergy, Asthma & Immunology. Symptoms? Swelling in the throat, trouble breathing, hives, rapid pulse, or a sudden drop in blood pressure. This is an emergency. Call for help immediately.Other immediate reactions include acute hives, wheezing, or a sudden rash. Penicillin and other antibiotics are common triggers. In fact, 73% of penicillin-related anaphylaxis cases occur within 15 minutes of dosing. If you’ve had a reaction before, your doctor may ask you to wait in the clinic for 30 minutes after your first dose. Don’t skip this. It’s not overcaution-it’s lifesaving.
Early Delayed Reactions: 1 to 72 Hours
Many side effects don’t show up right away but still come fast. Between one and three days after taking a drug, you might notice symptoms like mild rash, fever, joint pain, or nausea. These are often not allergies but your body’s response to the chemical. For example, some people develop a drug-induced fever or swollen lymph nodes within 24 to 48 hours after starting antibiotics like sulfonamides or anticonvulsants.According to Vinmec Medical Center, 92% of mild drug allergy symptoms appear in this window. It’s still early enough that stopping the drug can prevent things from getting worse. If you feel unwell but aren’t struggling to breathe, call your doctor within 24 hours. Don’t wait for it to get worse. This is also the window where drug-induced liver injury can begin-sometimes with just fatigue or yellowing skin. Don’t ignore it.
Delayed Reactions: 4 Days to 8 Weeks
This is where things get tricky. Most people assume side effects show up right away. But many of the most serious ones take weeks to appear. The most common? Maculopapular rashes. These are flat, red spots that spread across your chest, back, or arms. They usually show up between days 4 and 14, with a median of 8 days after starting antibiotics like amoxicillin or antivirals.Even more concerning is DRESS syndrome-Drug Reaction with Eosinophilia and Systemic Symptoms. It’s rare, affecting about 1 in 1,000 people on certain drugs like carbamazepine or phenytoin. But it’s deadly if missed. Symptoms include fever, swollen glands, liver problems, and a widespread rash. The median onset? 28 days. That’s almost four weeks after you started the medication. The FDA and NCBI Bookshelf both confirm that patients on these drugs need to be monitored for at least 8 weeks.
Other delayed reactions include drug-induced lupus (joint pain, fatigue, rash) and certain types of kidney injury. These can take weeks to months to develop. If you’ve been on a new medication for more than two weeks and suddenly feel off-tired, achy, or feverish-don’t assume it’s a cold. It could be your body reacting.

Chronic Reactions: Beyond 8 Weeks
Some side effects are slow burners. They don’t show up until you’ve been taking the drug for months. Statins like atorvastatin can cause muscle pain or weakness after 7 to 10 days in some people-but for others, the damage builds slowly. Interstitial lung disease from amiodarone? That can take 6 to 12 months to develop. It starts with a dry cough and shortness of breath, which many mistake for aging or asthma.Antidepressants are another classic example. You might not feel worse right away, but emotional blunting, weight gain, or sexual dysfunction often appear between day 14 and day 28. A meta-analysis in the Journal of Clinical Psychiatry found that 68% of these delayed side effects show up by day 21. That’s why doctors ask you to come back at two and four weeks after starting an antidepressant. It’s not a formality-it’s a critical checkpoint.
What Changes the Timeline?
Not everyone reacts the same way. Your body’s unique biology can speed up or slow down side effects. Age matters. People over 65 tend to experience side effects 2.3 days later than younger adults because their metabolism slows down. Kidney or liver problems? That delays drug clearance. A 2023 Mayo Clinic study found that patients with impaired kidney function see side effects last 30-50% longer.Genetics play a huge role. If you carry the HLA-B*57:01 gene, taking abacavir (an HIV drug) can trigger a severe reaction within 48 hours-with 99% certainty. That’s why doctors test for it before prescribing. Even something as simple as switching from a brand-name drug to a generic can change timing. About 23% of patients report different side effect onset after switching, likely due to different fillers or how fast the pill dissolves.
Other conditions matter too. People with autoimmune diseases react 37% faster to new drugs, according to FDA data. And dosage? Higher doses mean faster reactions. If you’re on a high dose, side effects can appear within 24 hours-whereas at a normal dose, they might take days.
What Should You Do?
Knowing when side effects can appear helps you act smart. Here’s a simple plan:- First hour: Watch for swelling, breathing trouble, or hives. If they happen, go to the ER.
- First week: Check for rash, fever, nausea, or dizziness every day. Keep a note of when each symptom started.
- Days 7-28: Pay attention to fatigue, joint pain, dark urine, or skin changes. These are red flags for delayed reactions.
- After 8 weeks: If you’re still on the medication, stay alert for slow-developing issues like muscle pain, cough, or mood changes.
Keep a symptom journal. Write down the date, time, and what you felt. A 2021 study showed that patients who tracked symptoms with minute-level detail were far more likely to get the right diagnosis. And 63% of those who kept a journal could tell the difference between a drug side effect and something else-like the flu-compared to just 29% who didn’t.
When to Call Your Doctor
Not every side effect means you need to stop the drug. Many mild ones-like nausea or drowsiness-fade as your body adjusts. About 78% of mild reactions resolve within 3 to 5 days without stopping the medication.But if you have any of these, call your doctor within 24-48 hours:
- A rash that spreads or blisters
- Swelling of the face, lips, or tongue
- Unexplained fever lasting more than 48 hours
- Yellow eyes or skin
- Severe muscle pain or weakness
- Difficulty breathing or chest tightness
For DRESS or other severe delayed reactions, starting corticosteroids within 48 hours can cut the death risk from 10% to just 2.3%. Timing saves lives.
The Future: Predicting Reactions Before They Happen
Doctors are getting better at predicting who will react and when. Mayo Clinic’s Personalized Medicine Program now uses algorithms that combine your genetics, age, kidney function, and medication history to forecast your side effect timeline with 84% accuracy. AI tools like IBM Watson analyze millions of past cases to spot patterns.Real-world tools are already helping. Patients using medication apps that track side effects report 32% fewer emergency visits. That’s not magic-it’s awareness. When you know what to watch for and when, you’re not just a patient. You’re an active partner in your care.
The bottom line? Side effects aren’t random. They follow patterns. And when you understand those patterns, you can act before things get dangerous.
How soon after taking a pill can side effects start?
Side effects can start as quickly as minutes after taking a pill-especially with allergic reactions like anaphylaxis, which often begin within 15 minutes. Other side effects, like rashes or nausea, may appear within 1 to 72 hours. Delayed reactions, such as DRESS syndrome or drug-induced lupus, can take weeks to show up. Even chronic side effects from drugs like statins or antidepressants may not appear until after several weeks or months of use.
Do all medications have side effects that appear at the same time?
No. Different drugs have different timelines. Over-the-counter pain relievers like ibuprofen often cause stomach upset within 30 minutes to 4 hours. Antidepressants usually take 2 to 4 weeks for side effects like weight gain or sexual dysfunction to appear. Antibiotics can cause rashes in 4 to 14 days. Drugs like carbamazepine or phenytoin may trigger life-threatening reactions like DRESS syndrome 2 to 8 weeks after starting. Timing depends on the drug, your body, and your genetics.
Can generic drugs cause side effects at different times than brand-name ones?
Yes. While the active ingredient is the same, generics can have different fillers, coatings, or dissolution rates. These differences can affect how quickly the drug enters your bloodstream. A 2022 study found that 23% of patients reported different side effect onset times after switching from brand-name to generic versions. If you notice a change in how you feel after switching, tell your doctor.
Should I stop my medication if I get a side effect?
Don’t stop without talking to your doctor. Many side effects-like mild nausea or drowsiness-are temporary and fade within a few days. Stopping abruptly can be dangerous, especially with antidepressants, blood pressure meds, or seizure drugs. But if you have signs of a serious reaction-rash with fever, trouble breathing, swelling, or yellow skin-stop the drug and seek help immediately. Your doctor will help you decide whether to stop, switch, or adjust the dose.
How can I tell if my symptoms are from the drug or something else?
Track your symptoms. Write down exactly when they started, what they feel like, and whether they worsen after taking your medication. People who keep a symptom journal are 63% more likely to correctly identify drug side effects than those who don’t. If your symptoms began shortly after starting the drug and improve after stopping it, that’s a strong clue. But always confirm with your doctor-some conditions, like infections or autoimmune flares, can mimic drug reactions.
Are older adults more likely to have delayed side effects?
Yes. Older adults metabolize drugs more slowly due to reduced liver and kidney function. Studies show they experience side effects an average of 2.3 days later than younger people. They’re also more likely to take multiple medications, increasing the risk of interactions. That’s why doctors often start seniors on lower doses and monitor them more closely.
What’s the most dangerous delayed side effect to watch for?
DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms) is one of the most dangerous. It can start 2 to 8 weeks after taking a drug like carbamazepine or allopurinol. Symptoms include high fever, rash, swollen lymph nodes, and organ damage-especially to the liver. Without prompt treatment, mortality can reach 10%. But if corticosteroids are started within 48 hours of recognizing symptoms, the death rate drops to 2.3%. Early detection is critical.
Can genetic testing predict when I’ll have a side effect?
Yes, for some drugs. Testing for the HLA-B*57:01 gene can predict with 99% accuracy whether someone will have a severe reaction to abacavir within 48 hours. Other genetic markers, like CYP2C19 variants, can predict how fast clopidogrel causes side effects. While not yet routine for all medications, genetic testing is becoming more common-especially for antidepressants, blood thinners, and seizure drugs. Ask your doctor if testing is right for you.
Next Steps: What to Do Right Now
If you’re starting a new medication:- Ask your pharmacist or doctor: “What side effects should I watch for, and when are they most likely to appear?”
- Write down the date you started the drug and keep a simple log of how you feel each day.
- Know the emergency signs: trouble breathing, swelling, fever with rash, yellow skin.
- Don’t ignore mild symptoms in the first week-they can be early warnings.
- Attend all follow-up appointments. They’re not optional.
Side effects aren’t a failure of the drug-they’re a signal. And when you know what to look for and when, you’re not just waiting for something to go wrong. You’re taking control.

