Warfarin-Antibiotic Safety Checker
Is Your Antibiotic Safe with Warfarin?
Check antibiotic interactions and get monitoring recommendations based on current medical guidelines
Results for
Risk Level
Why this matters:
Key Monitoring Instructions:
What to watch for:
Signs of bleeding include: unexplained bruising, blood in urine or stool, nosebleeds that won't stop, headaches that feel different, or unusual swelling.
When you’re on warfarin, even a simple antibiotic can turn into a silent danger. It’s not the infection you need to worry about-it’s what the antibiotic does to your blood thinning. Warfarin keeps your blood from clotting too easily, but it only takes a small shift in your body’s chemistry to push your INR too high. And when that happens, the risk of dangerous bleeding skyrockets. This isn’t rare. In fact, antibiotics are behind 15-30% of all warfarin-related hospital visits. The problem isn’t that antibiotics are bad. It’s that they mess with your body in ways most people don’t expect.
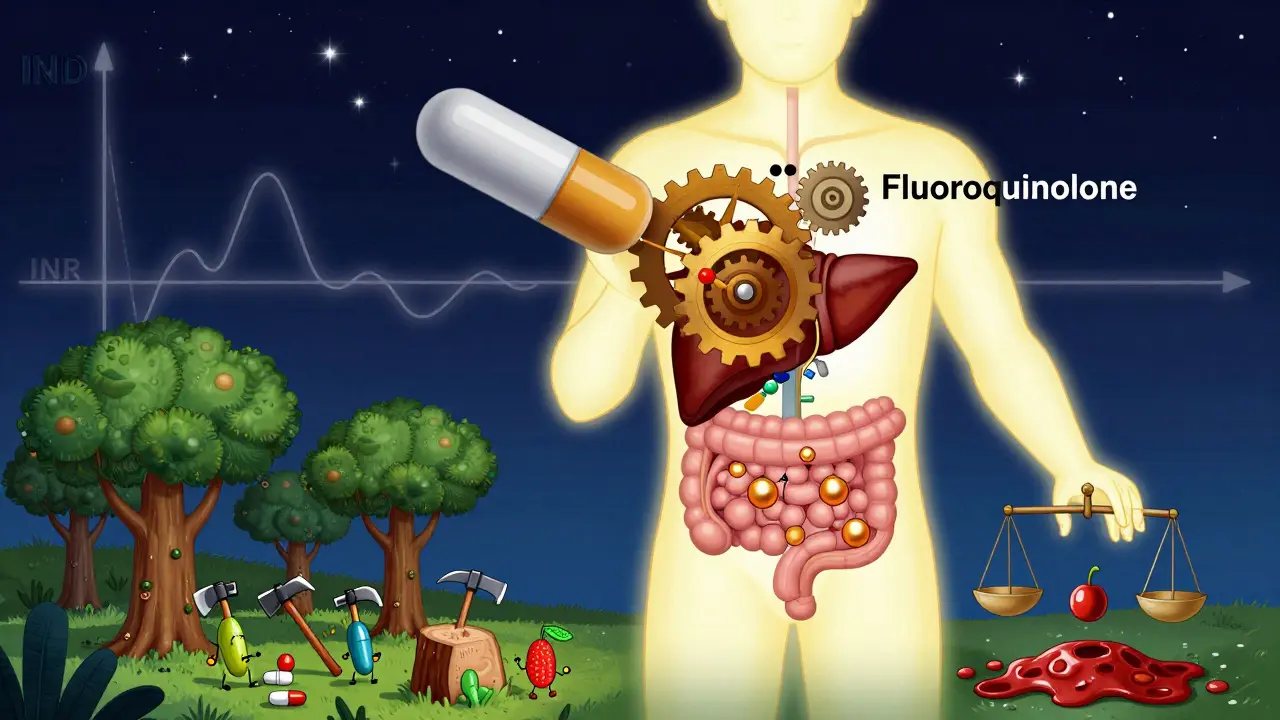
Why Antibiotics Change Your INR
Your INR measures how long it takes your blood to clot. For most people on warfarin, the target is between 2.0 and 3.0. Anything above 4.0 means your blood is taking way too long to clot-and that’s when bleeding becomes a real threat. Antibiotics don’t directly interact with warfarin like a chemical reaction. Instead, they disrupt two key systems in your body: your liver enzymes and your gut bacteria.Warfarin is broken down mostly by an enzyme called CYP2C9. Some antibiotics block this enzyme, causing warfarin to build up in your system. Others kill off the good bacteria in your gut that make vitamin K-a vitamin your body needs to make clotting factors. Less vitamin K means your blood thins even more. These two mechanisms work at different speeds. Liver enzyme changes happen fast-within 2 to 3 days. Gut bacteria disruption takes longer, usually peaking around day 5 to 7. That’s why bleeding risks don’t always show up right away.
Which Antibiotics Are the Riskiest?
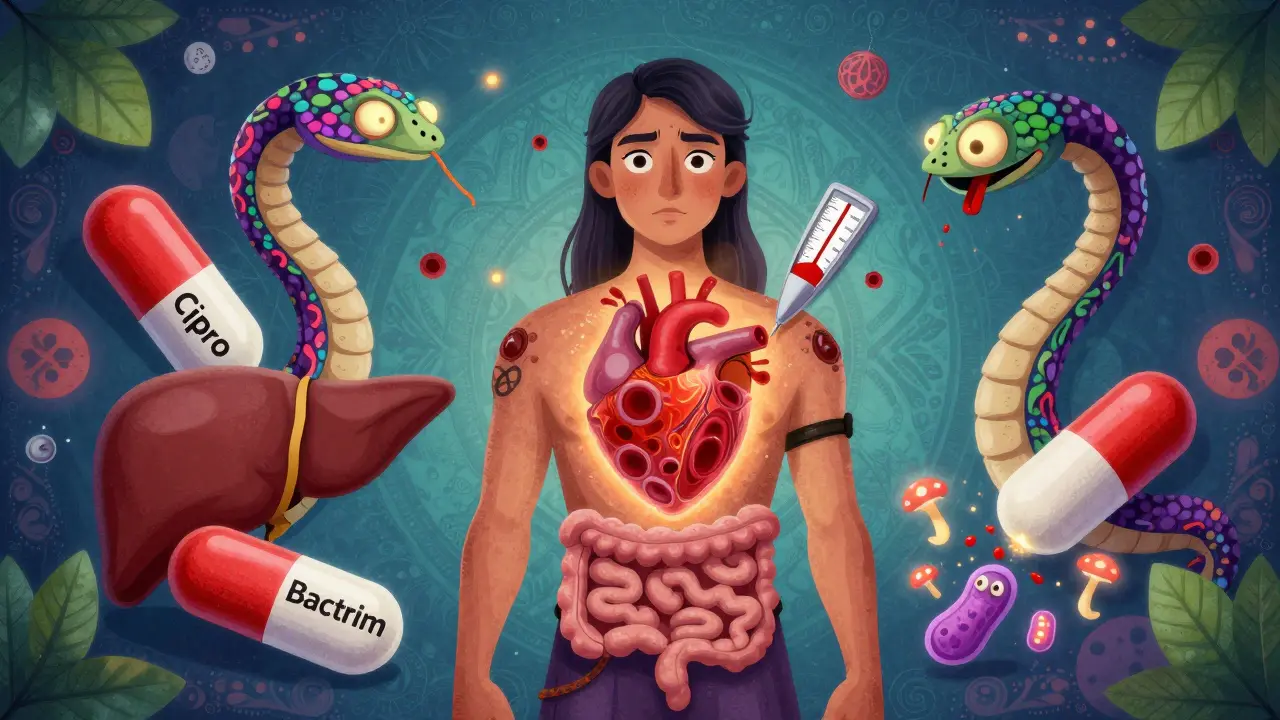
Not all antibiotics are created equal when it comes to warfarin. Some are low risk. Others are high risk. Here’s what the data shows:- High risk: Ciprofloxacin, levofloxacin (fluoroquinolones), erythromycin, sulfamethoxazole/trimethoprim (Bactrim), amoxicillin/clavulanate (Augmentin), cefotetan, and cefoperazone. These can push your INR up by 1.5 to 2.5 units on average.
- Moderate risk: Azithromycin (Zithromax), ceftriaxone. Azithromycin barely affects INR. Ceftriaxone causes small increases, usually under 0.5 units.
- Low risk: Nitrofurantoin, fosfomycin, and tedizolid. These rarely change INR and are often safer choices.
- Special case: Rifampin. This one does the opposite-it makes warfarin less effective. Your INR can drop below 1.5, putting you at risk for clots.
For example, if your INR is steady at 2.5 and you start ciprofloxacin, it’s common to see it jump to 4.1 within a week. That’s not a fluke-it’s a predictable reaction. A 2018 meta-analysis found ciprofloxacin increases bleeding risk by over 2 times. Bactrim? It raises INR by an average of 1.8 units in just 5 days. Even amoxicillin/clavulanate, which many doctors think is safe, can push INR up by 1.2 units. And here’s the kicker: you might not feel a thing until you start bleeding.
When Does the Risk Peak?
Most people assume the danger is highest when they first start the antibiotic. But the real danger window is between days 8 and 14. Why? Because that’s when the gut bacteria disruption kicks in fully. Your body has been slowly losing vitamin K production for days, and by day 8, it’s hit a tipping point. A 2012 study of over 31,000 Medicare patients found the risk of bleeding was more than 3 times higher during this period. Even after you stop the antibiotic, the risk doesn’t disappear right away. Gut bacteria take 7 to 10 days to recover. That means you still need to watch your INR for at least a week after finishing the antibiotic.
What Should You Do? A Clear Action Plan
You can’t avoid antibiotics if you need them. But you can control the risk. Here’s what works:- Get your INR checked before you start the antibiotic. Know your baseline. If it’s already near 3.0, you’re already on the edge.
- Check again within 72 hours of starting the antibiotic. For high-risk drugs like ciprofloxacin or Bactrim, don’t wait. Test early. If your INR jumps more than 0.5 units, your doctor may need to lower your warfarin dose by 20-30%.
- Test weekly until the antibiotic is done, then continue for another 7-10 days. Don’t assume stopping the antibiotic fixes everything. The gut bacteria take time to bounce back.
- Ask your doctor if a safer antibiotic is an option. If you have a urinary tract infection, nitrofurantoin is often just as effective as Bactrim-and doesn’t touch your INR. For pneumonia, azithromycin is a better pick than erythromycin.
- Know the signs of bleeding. Unexplained bruising, blood in urine or stool, nosebleeds that won’t stop, headaches that feel different, or any unusual swelling. Call your anticoagulation clinic immediately. Don’t wait.
Real-world data from GoodRx shows that 42% of warfarin-related ER visits happen because of antibiotics. Most of those cases could have been prevented with better monitoring. Pharmacist-led warfarin clinics reduce bleeding complications by 37% compared to doctor-only care. If your clinic doesn’t have a pharmacist on staff, ask if they can refer you to one.
What About Newer Antibiotics?
You might be thinking, “Are newer drugs safer?” The answer is yes-some are. Tedizolid, a newer antibiotic for skin infections, has been shown to cause almost no INR change. Fosfomycin and nitrofurantoin are also low risk. But don’t assume “new” means “safe.” Always check. The 2024 review in Expert Opinion on Drug Metabolism & Toxicology confirmed that even newer cephalosporins like cefotetan still carry a high risk. There’s no substitute for testing.