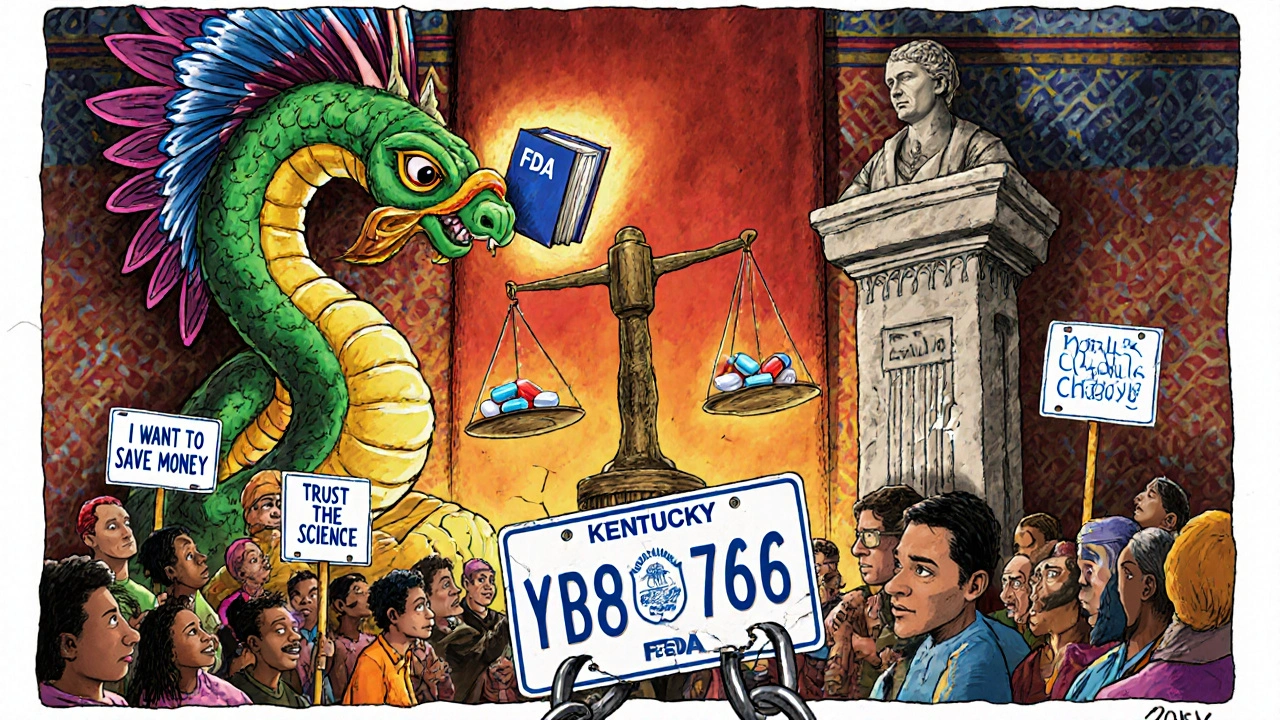
When you pick up a prescription for a drug like warfarin, levothyroxine, or phenytoin, you might assume the pharmacist can swap the brand name for a cheaper generic. But in many states, that’s not allowed - not because the generic doesn’t work, but because of state laws that treat these drugs differently. These are called NTI substitution laws, and they create a confusing patchwork across the U.S. that affects millions of patients every year.
What Are NTI Drugs and Why Do They Matter?
Narrow Therapeutic Index (NTI) drugs are medications where even tiny changes in dose can cause serious harm. A little too much, and you risk bleeding, seizures, or organ failure. A little too little, and the treatment fails completely. Examples include warfarin (a blood thinner), levothyroxine (for thyroid conditions), lithium (for bipolar disorder), and certain anti-seizure drugs like phenytoin and carbamazepine.
The FDA says approved generics are just as safe and effective as brand-name versions. They meet the same standards for bioequivalence - meaning the body absorbs them at the same rate and to the same extent. But some states don’t trust that. They’ve passed laws that either block substitution outright or add layers of paperwork, consent forms, and doctor approvals.
How States Differ: Three Main Rules
Not all states handle NTI drugs the same way. There are three main models:
- Carve-out laws: These states list specific NTI drugs that cannot be substituted at all. Kentucky, Pennsylvania, and North Carolina are examples. In Kentucky, pharmacists must check a 27-drug list before filling any prescription. If it’s on the list, they can’t switch - even if the patient asks.
- Affirmative consent laws: Here, the pharmacist must get written approval from both the doctor and the patient before making a switch. North Carolina requires this for refills. Connecticut goes further: if they substitute an anti-seizure drug, they must notify the doctor and patient within 72 hours. If either objects within 14 days, the swap is canceled.
- Notification-only laws: Pharmacists can substitute, but they must document it and send a notice to the prescriber. States like South Carolina and Minnesota use this approach. It’s less restrictive, but still adds administrative work.
Some states, like California, Texas, and Virginia, follow the FDA’s lead. They allow substitution without extra steps, trusting the approval process. That means a patient in Texas can get a generic warfarin without a second thought - but if they move to Kentucky, they might suddenly be stuck with the brand name, even if it costs three times more.
States With Strict NTI Substitution Rules
Here are some of the most restrictive states and what they require:
- Kentucky: Maintains a formal list of prohibited drugs - including digoxin, levothyroxine, lithium, and all strengths of warfarin sodium tablets. Substitution is only allowed if the prescriber writes a note saying it’s okay. Pharmacists say this adds 5 to 7 minutes per prescription.
- North Carolina: Requires written consent from both the prescriber and the patient for any NTI drug refill. These forms must be kept for three years.
- Pennsylvania: Has a legally binding list of NTI drugs. Pharmacists must verify each prescription against it. Violations can lead to fines or license suspension.
- Connecticut: Focuses on anti-epileptic drugs. Substitution triggers mandatory notification, and either the patient or doctor can block it within two weeks.
These rules aren’t just paperwork - they have real costs. A 2022 study found pharmacists in states with carve-out laws spend an extra 8.7 hours per month just on NTI compliance. Chain pharmacies use software that auto-checks state lists, but small, independent pharmacies often rely on manual checks. That means longer wait times and more stress for staff.

States With Fewer or No Restrictions
On the other end of the spectrum, states like California, Texas, Florida, and Virginia treat NTI drugs like any other generic. Pharmacists can substitute if the drug is listed as therapeutically equivalent in the FDA’s Orange Book. No extra forms. No doctor approvals. No delays.
That’s not because these states ignore safety. It’s because they trust the FDA’s evaluation. A 2020 study of over 12,000 Medicare patients on warfarin found no difference in bleeding risk between brand and generic versions. The American Heart Association used that data to argue against warfarin substitution bans.
California even passed a law in 2022 requiring its pharmacy board to base NTI designations on scientific reviews - not tradition. That’s a shift toward evidence, not fear.
Why the Conflict Exists
The tension between federal and state rules comes down to two things: science and control.
The FDA’s position is clear: if a generic passes bioequivalence testing, it’s safe to substitute. The agency doesn’t even officially label drugs as NTI - that’s a term used by clinicians, not regulators.
But state pharmacy boards argue they’re protecting patients. They point to case reports where switching brands caused INR levels to spike in warfarin patients or triggered seizures in people on anti-epileptics. Some of those cases are real. Others are anecdotal.
Experts are divided. Dr. Aaron Kesselheim from Harvard says state laws reflect real clinical concerns. “For warfarin, even a 10% difference in absorption can be dangerous,” he says. Meanwhile, the Generic Pharmaceutical Association argues that many drugs on state NTI lists aren’t even proven to have narrow therapeutic indexes. They say 35 of the 47 drugs on these lists lack solid evidence.
And then there’s the cost. NTI drugs account for $28.7 billion in annual prescriptions. States with strict substitution rules see 12.4% lower generic use. That means more money spent on brand-name drugs - and higher costs for patients, insurers, and Medicaid programs.
What’s Changing Now?
The landscape is shifting. In 2023, the FDA released draft guidance suggesting a clearer way to define NTI drugs - using a ratio of toxic dose to effective dose. Nine states, including New York and Ohio, are now reviewing their lists to align with this new standard.
The National Association of Boards of Pharmacy is also working on a model framework to bring some consistency across states. It’s expected by the end of 2025.
But change is slow. Kentucky’s NTI list is currently being challenged in federal court. The Association for Accessible Medicines argues it violates the Dormant Commerce Clause by making it harder for out-of-state generics to compete. If the court rules in their favor, it could force Kentucky and other states to rewrite their rules.
What This Means for Patients
If you take an NTI drug, here’s what you need to know:
- Check your state’s rules. If you move, your pharmacy might suddenly stop switching your meds.
- Ask your pharmacist: “Is this drug on my state’s NTI list?”
- If you’re switched to a generic, monitor for side effects. Even small changes can matter.
- If you’re happy with your brand-name drug, you can refuse substitution - in every state.
Some patients prefer staying on the same brand. Others want to save money. The law should give you a choice - but right now, it depends on where you live.
What Pharmacists Need to Do
Pharmacists are on the front lines. They have to know:
- Which drugs are restricted in their state
- Whether consent or notification is required
- How to document everything correctly
- When to refuse a substitution even if the patient asks
Many pharmacies use software that auto-flags NTI drugs based on location. But in smaller clinics or rural areas, staff still check printed lists or call the state board. It’s time-consuming - and error-prone.
The best practice? Always confirm the patient’s preference. Even in states that allow substitution, some patients have had bad experiences. Letting them choose builds trust - and avoids lawsuits.
Are all generic NTI drugs unsafe?
No. The FDA approves all generics based on strict bioequivalence standards. Studies show that for most NTI drugs, generic versions perform just as well as brand names. The concern isn’t that generics are unsafe - it’s that small differences in absorption could matter for drugs with very narrow safety margins. But evidence doesn’t consistently show higher risks with generics.
Can I request a brand-name NTI drug even if my state allows substitution?
Yes. Every state allows patients to refuse a generic substitution. You can ask for the brand name, and the pharmacist must honor it. Some doctors write "dispense as written" or "DAW 1" on the prescription to prevent substitution. That’s your right.
Why does Kentucky have such a long list of NTI drugs?
Kentucky’s list was built over decades based on clinical concerns and historical precedent, not recent scientific reviews. It includes drugs like levothyroxine and warfarin, which are widely used and have well-documented safety profiles. Critics argue the list is outdated and not based on current evidence. A federal lawsuit is now challenging its legality.
Do NTI substitution laws actually reduce adverse events?
Studies show states with carve-out laws report 28.7% fewer NTI-related adverse events, but that doesn’t prove the laws caused the drop. Other factors - like better monitoring, more patient education, or fewer substitutions overall - could explain the difference. No study has proven that blocking substitution directly prevents harm.
Will all states eventually stop restricting NTI substitutions?
It’s likely. As more data shows generics are safe, and as federal guidance becomes clearer, states are moving toward evidence-based rules. California’s 2022 law is a model for this shift. But because pharmacy regulation is a state power, full national uniformity is unlikely. Expect a mix of approaches for years to come.
What’s Next?
The future of NTI substitution laws depends on three things: science, lawsuits, and patient demand. If more studies confirm that generics are safe, pressure will grow to remove outdated restrictions. If courts strike down state lists as anti-competitive, more states will follow. And if patients start asking for generics - and saving money - pharmacies will push for change.
For now, the system is messy. But awareness is growing. Whether you’re a patient, a pharmacist, or just someone who takes medication, knowing your state’s rules could save you time, money, or even your life.

