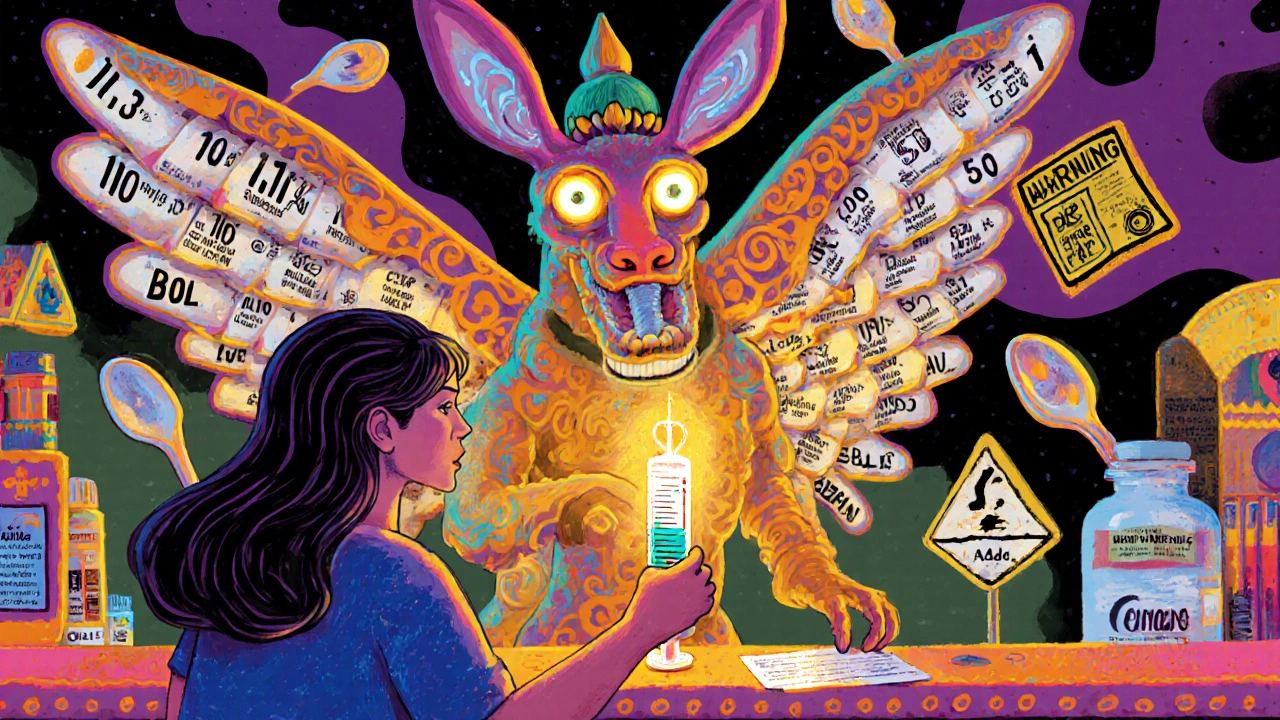
Dispensing Errors: What They Are, Why They Happen, and How to Stop Them
When a pharmacist gives you the wrong medicine, wrong dose, or wrong instructions, that’s a dispensing error, a preventable mistake in the final step of getting medication to a patient. Also known as pharmacy errors, these aren’t just paperwork glitches—they’re real risks that send people to the ER, cause permanent damage, or worse. Every year, over 1.3 million people in the U.S. are injured because of these mistakes, and many more go unnoticed because the harm is subtle—like a senior getting double the dose of blood pressure pills because the label got mixed up.
These errors don’t happen because pharmacists are careless. They happen because systems are stretched thin. Pharmacies fill hundreds of prescriptions a day. A similar-looking drug name—like Hydralazine and Hydroxyzine—can get misread in a rush. A barcode scan fails. A handwritten script is unclear. A patient gets the right drug, but the wrong strength because the label wasn’t double-checked. These are the quiet breakdowns that add up. And they’re often tied to bigger problems: understaffing, poor training, or lack of standardized safety checks. Medication errors, a broader category that includes prescribing and administration mistakes, are the third leading cause of death in U.S. hospitals. Prescription safety, the system of practices meant to prevent these mistakes isn’t just about technology—it’s about culture, communication, and clear processes.
You’re not powerless in this. The best defense is being an active participant. Always check the pill bottle against your prescription. Ask: "Is this what my doctor ordered?" Know the color, shape, and name of your meds. If it looks different, say something. Bring a list of everything you take to every appointment—including supplements. Ask your pharmacist to explain how each drug works and what to watch for. These simple steps cut your risk dramatically. And if you’ve ever seen a mislabeled bottle or heard a pharmacist say, "Oops, sorry," you know this isn’t rare. It’s systemic.
The posts below dig into real cases and solutions. You’ll find how NTI drugs like warfarin require extra care, why communication training in hospitals cuts errors, what questions to ask about drug interactions, and how to spot when a medication doesn’t look right. These aren’t theory pieces—they’re practical guides from people who’ve been there. Whether you’re managing multiple meds, caring for an elderly parent, or just trying to stay safe, this collection gives you the tools to catch mistakes before they hurt you.