When your shoulder aches after lifting groceries, or your knee burns after a long walk, it’s easy to blame it on "just getting older." But that pain might not be arthritis-it could be bursitis or tendinitis. These two conditions sound similar, and they often happen together, but they’re not the same. Knowing the difference isn’t just academic-it changes how you treat it, how fast you recover, and whether you risk making things worse.
What’s Actually Happening in Your Body?
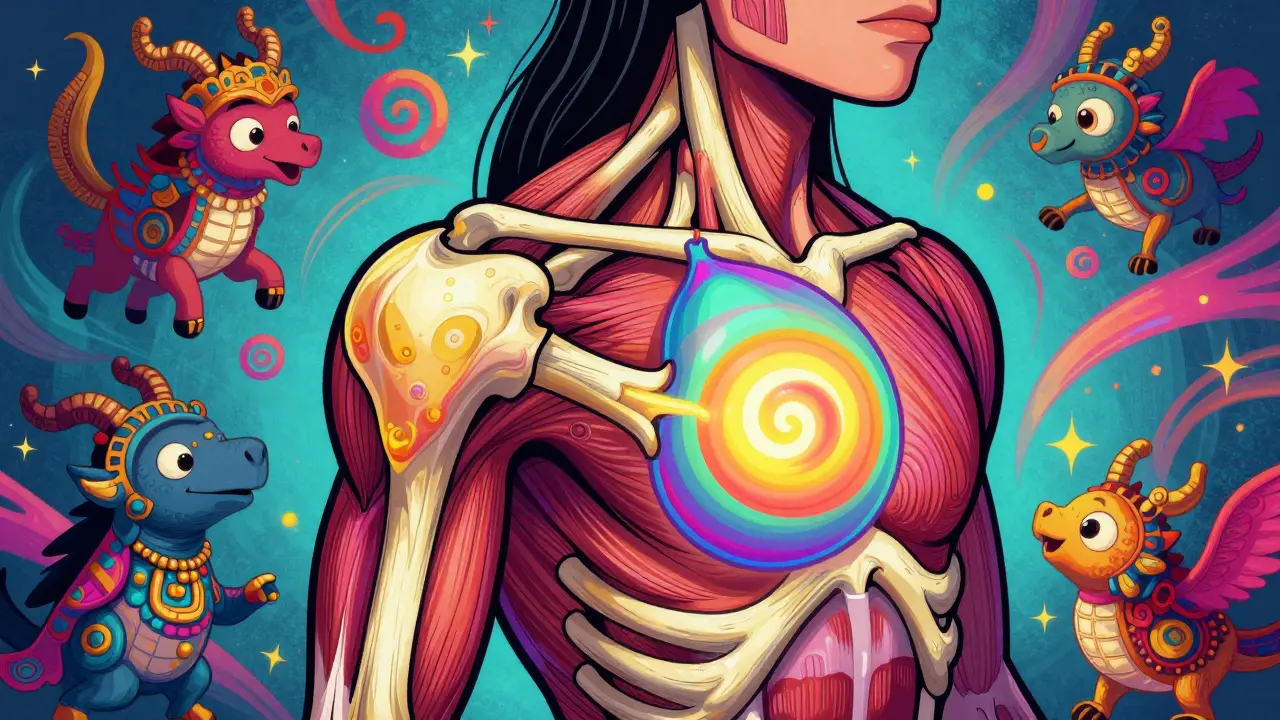
Bursitis is inflammation of the bursae. These are small, fluid-filled sacs that act like cushions between bones and the tendons or muscles that slide over them. There are about 160 of them in your body, but only a few get inflamed often-mostly around the shoulder, elbow, hip, and knee. When one of these sacs swells, it presses on nearby nerves and causes a dull, achy pain that gets worse when you lie on it or press on the joint.
Tendinitis, on the other hand, is inflammation of the tendons. These are the tough, rope-like tissues that connect your muscles to your bones. When you move, your muscles pull on these tendons to make your joints bend. If you repeat the same motion too much-like typing, painting, or swinging a tennis racket-the tendon gets irritated and starts to hurt. The pain usually follows the path of the tendon. For example, if your rotator cuff tendon is inflamed, you’ll feel pain when you lift your arm overhead.
Here’s the key: bursitis feels like pressure pain, while tendinitis feels like movement pain. If you’re in pain when you’re still, especially at night, it’s more likely bursitis. If it only hurts when you move a certain way, it’s probably tendinitis.
Where Do These Problems Usually Show Up?
Some spots are more prone to trouble than others. For bursitis, the top four trouble zones are:
- Shoulder (subacromial bursa) - common in people who reach overhead often, like painters or swimmers.
- Elbow (olecranon bursa) - often called "student’s elbow" or "miner’s elbow" from leaning on hard surfaces.
- Knee (prepatellar bursa) - common in gardeners or plumbers who kneel for hours.
- Hip (trochanteric bursa) - often mistaken for hip arthritis, especially in women over 40.
For tendinitis, the most frequent trouble spots are:
- Shoulder (rotator cuff tendons) - 31% of all tendinitis cases, according to the American Academy of Family Physicians.
- Elbow (tennis elbow or golfer’s elbow) - not just for athletes. Anyone who grips things tightly can get it.
- Knee (patellar tendon) - "jumper’s knee" from jumping sports, but also from climbing stairs or squatting.
- Ankle (Achilles tendon) - common in runners and walkers, especially if you suddenly increase your mileage.
And here’s something surprising: 65% of shoulder pain cases involve both bursitis and tendinitis at the same time. That’s why so many people get misdiagnosed. If your doctor treats only one, the other keeps causing pain.
How Do You Know Which One You Have?
Doctors don’t just guess. They use a few simple tests. First, they press on the joint. If the pain is centered over a soft, swollen bump, it’s likely bursitis. If the pain runs along a line from muscle to bone, it’s tendinitis.
Then they ask you to move. For shoulder tendinitis, you’ll feel sharp pain when you lift your arm sideways. For hip bursitis, lying on that side will wake you up at night. For Achilles tendinitis, you’ll feel stiffness in the morning that eases after walking a few steps.
Imaging isn’t always needed. But if the pain lasts more than a few weeks, an ultrasound can confirm the diagnosis with 92% accuracy. MRIs show more detail, but they’re expensive and often show inflammation in people who feel no pain at all. As Dr. Laura Robbins from the Hospital for Special Surgery says, "Forty percent of people over 50 have bursitis or tendinitis on an MRI-and they never knew it." So don’t trust scans alone. Your symptoms matter more.

What Actually Helps? (And What Doesn’t)
Most cases get better without surgery. But the treatment depends on which condition you have.
For bursitis: Rest, ice, and avoiding pressure on the area are the first steps. NSAIDs like ibuprofen help reduce swelling. If it doesn’t improve in a couple of weeks, a corticosteroid injection into the bursa can give you 78% relief within four weeks, according to the American Journal of Sports Medicine. That’s because bursae respond well to anti-inflammatory meds.
For tendinitis: Injections? Not so much. Only 52% of people get relief, and injecting a tendon can weaken it. The real fix is movement-specifically, eccentric strengthening. That means slowly lowering a weight after lifting it. For Achilles tendinitis, that’s doing heel drops: standing on a step, rising on your toes, then slowly lowering your heel below the step. Do 180 reps a day for 12 weeks. Sounds like a lot? It is. But 68% of people see lasting improvement, compared to just 41% with injections alone.
And here’s the thing: if you do the wrong thing, you’ll make it worse. A 2023 study in the Journal of Orthopaedic & Sports Physical Therapy found that patients who were told to stretch or strengthen an inflamed bursa ended up with symptoms lasting 3.2 times longer than those who got the right treatment.
What to Do at Home
You don’t need a clinic to start feeling better. Here’s what works based on real user reports from Arthritis Foundation forums and Reddit:
- Ice massage: Freeze water in a paper cup, peel back the top, and rub the ice over the painful area for 5-10 minutes. People rate this 4.2 out of 5 for shoulder and knee pain.
- Pain monitoring: During exercise, keep pain under 3 out of 10. If it hits 5 or higher, you’re pushing too hard. That’s the rule physical therapists use.
- Posture correction: Slouching at your desk strains your shoulders. Adjust your chair height so your arms are parallel to the floor. This helped 82% of people in an Arthritis Today survey.
- Modify your routine: If you play tennis, switch to a lighter racket. If you kneel at work, use a cushion. Even small changes cut flare-ups by half.
One Reddit user, a 58-year-old gardener with hip bursitis, said: "I started using a foam pad when I knelt. Within two weeks, the night pain was gone. No shots, no meds. Just better posture and less pressure."

When to See a Doctor
You don’t need to rush to the ER for either condition. But if you notice any of these signs, get checked:
- Fever or redness around the joint - could mean infection.
- Joint locking or popping - might mean a tear.
- Weakness in the limb - could signal nerve or tendon damage.
- Pain that doesn’t improve after 2-3 weeks of rest and ice.
Also, if you’ve had a cortisone shot before and it didn’t help-or made things worse-it’s time to dig deeper. Many people keep getting repeat shots because they’re told it’s "just bursitis," when the real issue is a torn tendon or muscle imbalance.
The Bigger Picture: Why This Matters
These aren’t just "old person problems." In 2022, over 387,000 U.S. workers missed time because of bursitis or tendinitis. That’s more than 11 million lost workdays. Construction workers, musicians, office workers, and athletes are all at risk.
And the cost? The global market for treating these conditions hit $4.7 billion in 2022-and it’s growing. Why? Because people are living longer and staying active. But many still treat them like temporary annoyances instead of signals to change how they move.
There’s new hope, too. Platelet-rich plasma (PRP) injections are showing better long-term results than cortisone for chronic tendinitis. Ultrasound-guided injections are now standard because they hit the target 95% of the time, not 70%. And wearable tech like the Apple Watch is being tested to detect risky movement patterns before pain even starts.
But the most powerful tool isn’t high-tech. It’s awareness. Knowing whether it’s your bursa or your tendon that’s inflamed changes everything. It means you stop guessing. You stop taking shots that don’t help. You start doing the right exercises-and finally, you start feeling better.
Frequently Asked Questions
Can bursitis and tendinitis happen at the same time?
Yes, and they often do. In fact, 65% of shoulder pain cases involve both conditions. The bursa and tendon sit right next to each other, so irritation in one often spreads to the other. That’s why treating only one part usually leads to incomplete recovery. A good doctor will check both.
Are cortisone shots safe for tendinitis?
They’re risky. While cortisone reduces swelling, it can weaken tendons over time, increasing the chance of a tear. Studies show only 52% of tendinitis patients get short-term relief, and long-term outcomes are worse than with exercise. For bursitis, injections are much more effective and safer. Always ask your doctor if the injection is meant for the bursa or the tendon.
How long does it take to recover from tendinitis?
It takes longer than most people expect. Bursitis often improves in 4-6 weeks with rest and anti-inflammatories. Tendinitis? Not so fast. For chronic cases, especially in the Achilles or shoulder, you need 12-16 weeks of consistent eccentric strengthening. Rushing back to activity too soon is the #1 reason people relapse.
Is "tendinitis" the right term anymore?
Many experts now prefer "tendinopathy" because chronic cases aren’t always inflamed-they’re degenerated. The tissue breaks down from overuse, not just irritation. That’s why anti-inflammatories don’t always work. The focus has shifted from reducing inflammation to rebuilding tendon strength through controlled loading.
Can I prevent bursitis and tendinitis?
Yes. Avoid repetitive motions without breaks. Use cushions when kneeling. Warm up before activity. Strengthen the muscles around your joints. And listen to your body-if something hurts during movement, stop and adjust. Small changes in how you move can prevent years of pain.